|
Our bones are remarkable examples of evolution's ingenuity. From a functional perspective, bones serve multiple roles - structure, mobility, support, protection as well as serving as a reservoir for essential minerals. These roles became important, when our distant predecessors left the calcium-rich ocean to live in calcium-poor fresh water, and then further evolved to live on land where gravitational forces (without the buoyancy effect of water) put greater stress on the skeleton. Our skeletons store two key minerals, calcium and phosphorus, both essential for the healthy functioning of cells and bodily organs, and our bones are called, in times of stress, to maintain blood levels of both.
A complex system of hormones regulates calcium and phosphorus in our bodies acting on bone, intestine and kidneys to maintain adequate supply for proper cellular function in all cells but particularly in nerves and muscle. These hormones include: Calcium Regulating Hormones
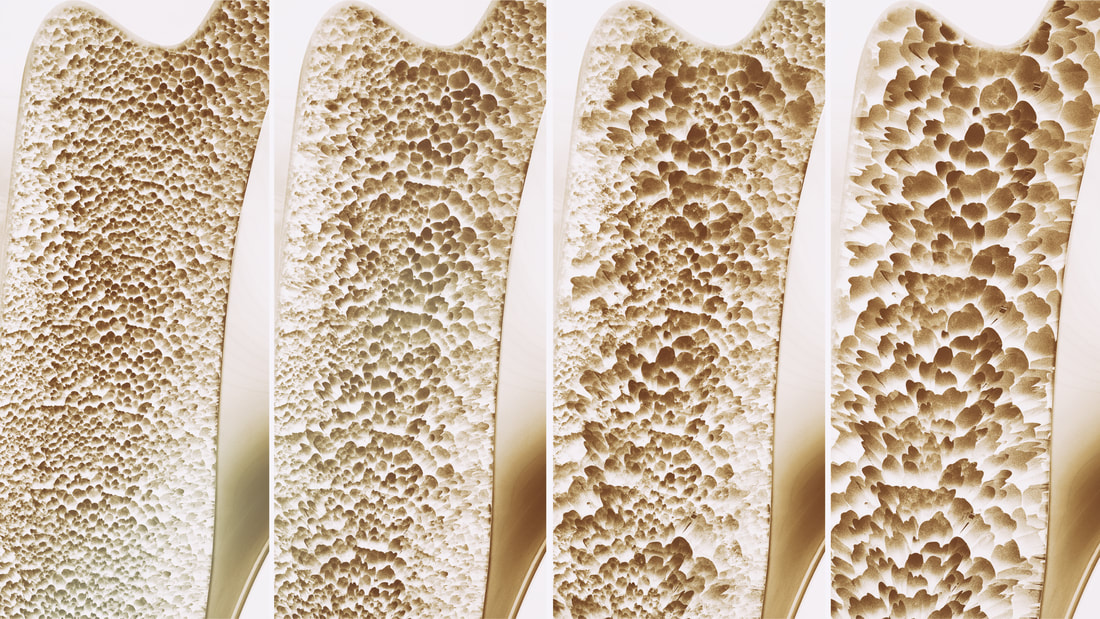
Of these, Vitamin D stands out, as we are dependent on our environment, specifically sunlight to synthesize adequate Vitamin D to maintain adequate dietary calcium absorption from our intestines. The dual roles of bone, to act as structure and at the same time represent a reservoir for calcium and phosphorus, are in direct conflict with each other. Bones must be strong and flexible to respond to the weight bearing and mechanical forces of our activities. When our activities increase in intensity, our bones get stronger in order to sustain the load. However if calcium or phosphorus are in short supply, our regulatory hormones will draw them out of bone to serve vital functions in other cells in the body, and in the process potentially weaken bone. Bone is an incredible material providing both strength and flexibility in order to be resilient to the mechanical forces imposed by daily activities, not to mention sports. To accomplish this bone is a composite material made of minerals bound to protein, predominantly collagen. If bone was made only from mineral crystals it would be brittle and fracture easily; if made solely from protein it would be too flexible and would not provide adequate structure and flexibility. The mineral components of bone are crystals of calcium and phosphate called hydroxyapatite. They are bound in a matrix to a triplet of three long, thin, intertwined collagen rods with are strengthened by chemical bonds between proteins. Other proteins further strengthen the collagen matrix and regulate mineral binding. Small changes in shape of the bones, from mechanical forces, act on the cells inside the bone to send signals that allow bone to respond to these loads by remodelling and strengthening. In this way, our bones are always changing and growing, responding to mechanical loads, resorbing and laying down new bone. Bone health depends on the balanced effects of two kinds of bone cells:
Once growth is finished and we are adults, osteoblasts spend less time creating new bone and more time regulating bone repair - osteoblasts signal osteoclast to hollow out bone in a specific location and then fill in that area with new & healthy bone. Bone also has another remarkable feature - it is anti-fragile: if stressed it gets stronger. This phenomena, called Wolff's Law was originally recognized in late 19th century, but is probably most dramatically visualized in tennis players who show far greater bone mass in their racket arm as compared to their non-dominant arm. This remarkable gift, that our bones grow stronger through stress and usage has a dark, flip side: our bones grow weaker through disuse. Only in modern times has this become a downside. For most of human history, our lives were simply too active. Our predecessors had very strong bones from all the physical work and stress placed on their bones throughout their lives. From the industrial revolution on onward, labor saving technologies have decreased the degree to which we need to use our bodies to the point that many of us are no longer building enough bone. This is another example of evolutionary mismatch that I have previously written about. Compounding this fundamental mismatch, modern diets and lifestyles also lead to deficiencies in dietary calcium, protein and Vitamin D necessary for bone health. To develop and maintain bone mass three key principles emerge:
Next week, we will look at osteoporosis and what you can do to prevent or reverse it. Today I am going to provide a list of 7 biomarkers for you health - numbers you should know. These are all biomarkers that can be improved through lifestyle interventions - they are numbers that can be normalized and optimized - and in doing so you will reduce your risk for heart disease, diabetes, cancer, Alzeimher's dementia, kidney failure, arthritis and many other conditions. Optimizing these biomarkers will even decrease your risk of premature death. I think this should be a pretty good investment of 15 minutes of reading! (If you want to skip the reading - there is a quick summary at the end of this post).
2. Gamma Glutamyl Transferase (GGT) - optimal < 30 U/L GGT measures a liver enzyme and is commonly described as liver function test most closely associated with the adverse effect of alcohol. GGT is however much more important as it is an indirect measure of the body’s glutathione supply. Glutathione protect cells against the oxidative stress resulting from metabolism. Without this protection the free radicals generated by mitochondria through normal metabolism with oxygen would accumulate, overwhelm and damage the mitochondria and the cell. In normal ageing it has been shown that it is this accumulation of oxidative stress that leads to many of the age-related diseases. In many ways, glutathione is consider the master antioxidant: working with as part of the enzyme glutathione peroxidase to protect membranes from oxidation, enabling Vitamin E and C in their anti-oxidant capacities as well as working directly. Glutathione is also a key component of the Phase II metabolism (detoxification) of drugs, hormones and xenobiotics where it works as a component of an enzyme Glutathione s-transferase (GST) that conjugates heavy metals, toxins and other compounds so that they become water soluble and can be excreted in the bile or urine. Exposure to high levels of toxins that overwhelm glutathione in its Phase II metabolic role will lead to oxidative stress. 3. hsCRP - high sensitivity CRP - optimal < 1.0 Again another topic I have recently blogged about: chronic inflammation. Chronic inflammation is at the root of 7 of the top 10 causes of death accounting for 80% of all deaths in our society. The most insidious aspect of this type of inflammation is its silent nature that allows for damage to occur without diagnosis. HsCRP is the gold standard for assessing chronic inflammation - optimizing this number through behavioural change - diet, exercise, stress reduction - decreases the risk for many diseases. 4. Blood Pressure - optimal <115/75 (systolic/diastolic pressures measured in mmHB) This is the simplest - something that you can do at home, at the local pharmacy and with your doctor. Normal blood pressure is 120/80. Recently there were major headlines in the US, noting a change in the definition of high blood pressure (hypertension), lowering the definition threshold to 130/80 from 140/90. While this change dramatically increases the number of people who will be diagnosed with hypertension - not all will automatically be recommended medications. Those recommendations will depend on a person’s overall risk for cardiovascular disease - anyone with a 10% or greater risk should aim to bring the BP below 130/80. High blood pressure or hypertension is quantitatively the most important modifiable risk factor for cardiovascular disease (the largest contributor to premature death in our society). It is also a significant risk factor for both kidney and heart failure. For every 20 mmHg increase in diastolic blood pressure above 75, the risk of death from heart disease or stroke doubles. Elevations in blood pressure are caused by dysfunctions within core biological systems
5. Fasting Blood Glucose and or HbA1c: optimal FBS <5.2mmol/L (normal <5.6 mmol/L); optimal HbA1c <5.0% Maintaining normal blood sugars is one of the most important and tightly regulated functions in your body. Diabetes mellitus (DM) is the condition when your body cannot maintain normal blood glucose levels. Type I DM is an autoimmune disease where the pancreas stops producing insulin. Type II DM, is characterized by insulin resistance, where the body no longer responds normally to insulin. In order to maintain blood sugars, the pancreas increases production of insulin - leading to elevated insulin levels which in turn trigger inflammatory changes, which in a vicious cycle further worsens insulin resistance. Insulin resistance precedes Type II Diabetes and can remain undetected for years, as glucose levels are maintain as normal until the pancreas begins to fail, which is relatively late in the process. Diabetes is diagnosed when FBS >7.0 or HbA1c >6.5% Type II DM is currently at epidemic levels globally having tripled since 2000. Almost 500M people or 1 in 11 have diabetes at an estimated cost of $850M. The direct complications from diabetes come from damage to blood vessels at two levels:
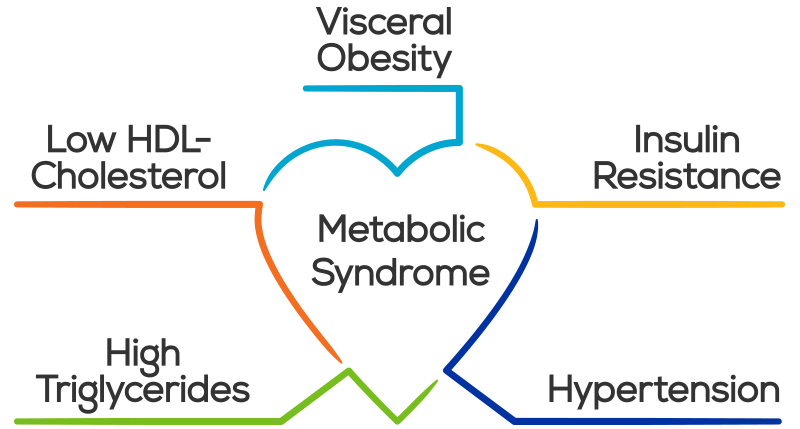
6. TG/HDL - Triglyceride/HDL ratio - optimal <1.0 Of all the information that can be derived from a lipid panel the TG/HDL ratio provides the best information about risk. TG/HDL is an excellent marker for insulin resistance and metabolic syndrome When elevated above 3.5 - this is the simplest test to identify atherogenic dyslipidemia, which is marked by the joint occurrence of elevated TG, low HDL and atherogenic, small, dense, LDL particles. This is highly predictive of cardiovascular disease. As we have seen above insulin resistance is the precursor to Type II DM and is often silent and undiagnosed, and is also one of the major causes of chronic inflammation. 7. Android:Gynecoid Fat Ratio - optimal <1.0 The major cause of the global diabetes epidemic is the associated obesity epidemic. Over 2B people are overweight with about 600M reaching the definition of obese (BMI >30). For obese people cardiovascular disease is the leading cause of death and disability, followed by diabetes. Kidney failure and cancer are the other major causes of death. Obesity, through adipocyte dysfunction leads to a chronic inflammatory state that predisposes an individual for many diseases. Abdominal or visceral fat contributes disproportionately to this inflammatory response as compared to peripheral fat. The best way to measure visceral fat is with a DXA body scan, which provides you with android:gynecoid fat ratio. The ratio correlates with insulin resistance, showing the clear link between visceral fat and the pathogenesis of diabetes. The added benefit of getting a DXA scan is getting understanding your lean muscle mass and bone density. As you age maintaining lean body mass and bone density are both essential for vital longevity avoiding age-related sarcopenia and osteoporosis. A good alternative (without the extra bone and lean body information) is a waist:hip ratio. The optimal ratio for men in <0.85 and women <0.75. Abdominal obesity is also a marker for metabolic syndrome - a cluster of conditions that carry risk individually but are collectively carry massive risk:
As you can see, all of the risks for metabolic syndrome have been covered by our 7 numbers.
According to a recent study - almost 1 in 5 Canadians, including 40% of people over 65 have metabolic syndrome . Unfortunately, many are unaware of it and have placed themselves at massively increased risk for diabetes, heart disease and premature death. In Summary - 7 Numbers You Should Know
It's that time of year again in Canada, days are short and still getting shorter, light is fleeting and we are talking about Vitamin D. In this post, I am going to answer the questions we get about Vitamin D:
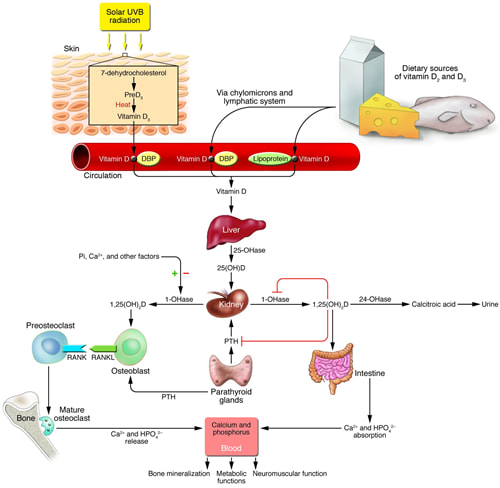
Vitamin D, the “sunshine vitamin", is a powerful hormone that your body makes through exposure to sunlight. From an evolutionary perspective Vitamin D is one of the oldest hormones found in biology, first appearing over 500 million years ago as a cellular factor protecting proteins, DNA and RNA from UV light damage. As organisms ventured from the oceans to land, a mechanism to obtain adequate calcium was necessary to maintain vertebrate skeletons. Calcium is abundant in oceans but on land, it is locked in soil and only available to plants. Vitamin D, synthesized in response to sunlight, evolved to ensure the intestinal absorption of calcium. For many years, this was what we understood about Vitamin D: that it is essential for proper calcium metabolism and bone health. Deficiencies in Vitamin D leads to rickets, the childhood disease of bone weakness, bowed femurs and tibias. Supplementing with dietary sources of Vitamin D to prevent rickets goes back to the early 1800’s with the use of cod liver oil (high in Vitamin D) and became mainstream in the 1930’s when milk was fortified with Vitamin D. Vitamin D Physiology Vitamin D3 (cholecalciferol) the hormone precursor is synthesized from 7-dehydrocholesterol in the skin in response to ultraviolet B (UVB) rays. UVB rays are present only during midday at higher latitudes and do not penetrate clouds. The time needed to produce adequate vitamin D from the skin depends on the strength of the UVB rays, the length of time spent in the sun, and the amount of pigment in the skin. At our northern latitude, UVB strength is not adequate from October to March so we must supplement. Very few foods naturally contain significant amounts of vitamin D (fish, shiitake mushrooms being exceptions) so obtaining adequate Vitamin D from non fortified food alone is difficult. Even with food fortification, it is thought that most Canadians have insufficient Vitamin D levels for optimal health. From production in the skin, Vitamin D binding protein transports Vitamin D3 to the liver where it undergoes hydroxylation to 25(OH)D - the half-life of this Vitamin D pro-hormone in the liver is 3 weeks. 25(OH) D is transported from the liver to the kidney where it is hydroxylated by 1 alpha hydroxylase (CYP27B1) to 1,25(OH) 2 D - the active form of Vitamin D. Both 25(OH)D and 1,25 (OH) 2 D are degraded by 24-hydroxlase (CYP24A1). Vitamin D then acts on the intestine to increase the absorption of calcium, on the bone to increase bone resorption and increase blood levels of calcium and on the kidney to decrease calcium and phosphate excretion. Vitamin D’s role in calcium physiology is clear and several meta-analyses have shown that supplementation with Vitamin D and calcium decrease the risk of osteoporotic fractures in older people. More recent research has shown that Vitamin D regulates many other cellular functions:
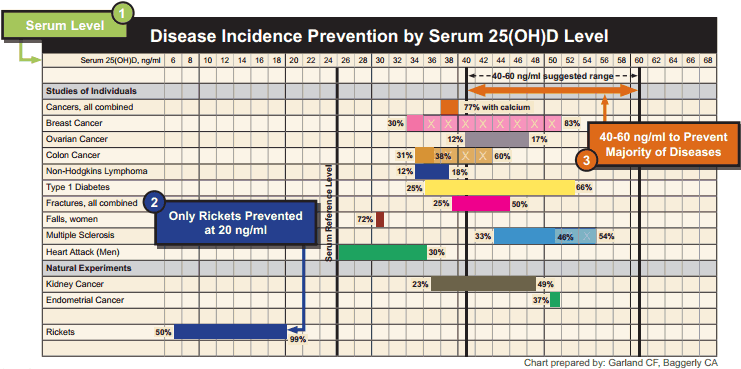
An explosion of research has suggested the Vitamin D may prevent or be useful in treating more than 100 disorders, ranging from:
All this evidence makes one thing clear - blood levels of Vitamin D are a good indicator of health across many conditions; what is less clear is whether low levels of Vitamin D cause poor health outcomes or whether the poor outcomes themselves can decreases in Vitamin D. The only way to determine this is through well designed double-blind supplementation trials, which are expensive and difficult to do properly. Still for many of these conditions trials are underway to determine the potential causal role of Vitamin D in many conditions. There are many factors that lead to signifiant variation in blood levels of Vitamin D:
So at this point we have established:
So the next question is how much Vitamin D should I take? This is where things get a bit controversial. If we look at disease association data, the optimal Vitamin D 25(OH)D blood levels appears to be between 100 - 150 nmol/L (40-60 ng/ml) The venerable Institute of Medicine (IOM) stated in their 2010 guidelines that levels of 50 nmol/L ( 20 ng/ml) are adequate. At Wellness Garage, we are most comfortable when clients are in the 100 - 150 nmol/L (40-60 ng/ml) and recognize that levels of >200 nmol/L (80ng/ml) are potentially toxic. So how much Vitamin D do you have to take to reach this level? Again this is controversial… The IOM bumped its recommended dietary intake from 400 to 600 IU for adults and for 800 IU for age >70 years. The maximum level was set at 4000 IU. Many, including us at Wellness Garage, think these recommendations are low. For those who have not been tested for Vitamin D, we recommend 2000 IU per day. For anyone taking doses greater than 5000 IU we also recommend testing. For those who can afford testing, we recommend getting tested during the winter December to February and adjusting your supplementation based on the results. Vitamin D testing is no longer a medically insured service in most parts of Canada due to the cost, especially when a simple one size fits all recommendation to supplement will likely help most people. We think this makes sense from a public policy perspective, at least until there is better evidence to support that supplementation itself prevents or reverses disease. We do think that individuals who are looking to optimize their health should test as there are simply too many variables to ensure that a standard dose of Vitamin D will put you in the optimal zone AND we feel that while the causal role of Vitamin D has not been proven for most conditions, it is one of the most important health indicators and the potential benefit of optimizing Vitamin D levels outweigh the negligible risks with supplementation when guided by testing. So if you skipped over most of this to find the answers to your questions - here is a quick summary:
|
AuthorDr. Brendan Byrne Categories
All
|


 RSS Feed
RSS Feed