|
It's that time of year again in Canada, days are short and still getting shorter, light is fleeting and we are talking about Vitamin D. In this post, I am going to answer the questions we get about Vitamin D:
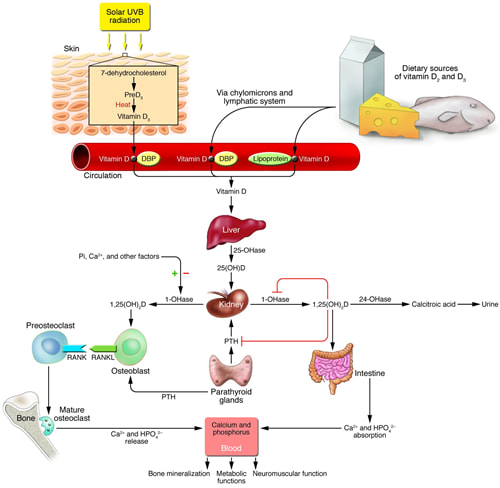
Vitamin D, the “sunshine vitamin", is a powerful hormone that your body makes through exposure to sunlight. From an evolutionary perspective Vitamin D is one of the oldest hormones found in biology, first appearing over 500 million years ago as a cellular factor protecting proteins, DNA and RNA from UV light damage. As organisms ventured from the oceans to land, a mechanism to obtain adequate calcium was necessary to maintain vertebrate skeletons. Calcium is abundant in oceans but on land, it is locked in soil and only available to plants. Vitamin D, synthesized in response to sunlight, evolved to ensure the intestinal absorption of calcium. For many years, this was what we understood about Vitamin D: that it is essential for proper calcium metabolism and bone health. Deficiencies in Vitamin D leads to rickets, the childhood disease of bone weakness, bowed femurs and tibias. Supplementing with dietary sources of Vitamin D to prevent rickets goes back to the early 1800’s with the use of cod liver oil (high in Vitamin D) and became mainstream in the 1930’s when milk was fortified with Vitamin D. Vitamin D Physiology Vitamin D3 (cholecalciferol) the hormone precursor is synthesized from 7-dehydrocholesterol in the skin in response to ultraviolet B (UVB) rays. UVB rays are present only during midday at higher latitudes and do not penetrate clouds. The time needed to produce adequate vitamin D from the skin depends on the strength of the UVB rays, the length of time spent in the sun, and the amount of pigment in the skin. At our northern latitude, UVB strength is not adequate from October to March so we must supplement. Very few foods naturally contain significant amounts of vitamin D (fish, shiitake mushrooms being exceptions) so obtaining adequate Vitamin D from non fortified food alone is difficult. Even with food fortification, it is thought that most Canadians have insufficient Vitamin D levels for optimal health. From production in the skin, Vitamin D binding protein transports Vitamin D3 to the liver where it undergoes hydroxylation to 25(OH)D - the half-life of this Vitamin D pro-hormone in the liver is 3 weeks. 25(OH) D is transported from the liver to the kidney where it is hydroxylated by 1 alpha hydroxylase (CYP27B1) to 1,25(OH) 2 D - the active form of Vitamin D. Both 25(OH)D and 1,25 (OH) 2 D are degraded by 24-hydroxlase (CYP24A1). Vitamin D then acts on the intestine to increase the absorption of calcium, on the bone to increase bone resorption and increase blood levels of calcium and on the kidney to decrease calcium and phosphate excretion. Vitamin D’s role in calcium physiology is clear and several meta-analyses have shown that supplementation with Vitamin D and calcium decrease the risk of osteoporotic fractures in older people. More recent research has shown that Vitamin D regulates many other cellular functions:
An explosion of research has suggested the Vitamin D may prevent or be useful in treating more than 100 disorders, ranging from:
All this evidence makes one thing clear - blood levels of Vitamin D are a good indicator of health across many conditions; what is less clear is whether low levels of Vitamin D cause poor health outcomes or whether the poor outcomes themselves can decreases in Vitamin D. The only way to determine this is through well designed double-blind supplementation trials, which are expensive and difficult to do properly. Still for many of these conditions trials are underway to determine the potential causal role of Vitamin D in many conditions. There are many factors that lead to signifiant variation in blood levels of Vitamin D:
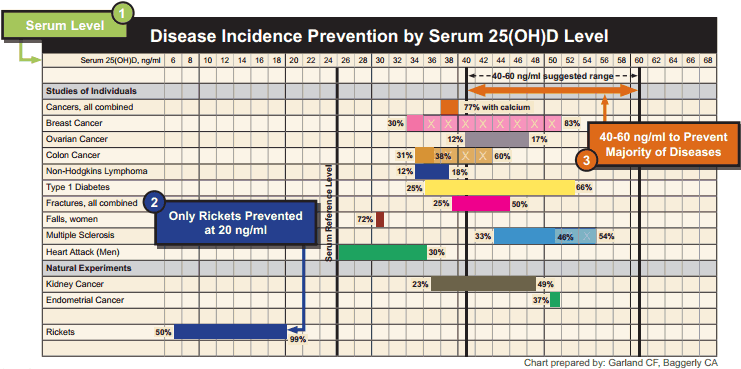
So at this point we have established:
So the next question is how much Vitamin D should I take? This is where things get a bit controversial. If we look at disease association data, the optimal Vitamin D 25(OH)D blood levels appears to be between 100 - 150 nmol/L (40-60 ng/ml) The venerable Institute of Medicine (IOM) stated in their 2010 guidelines that levels of 50 nmol/L ( 20 ng/ml) are adequate. At Wellness Garage, we are most comfortable when clients are in the 100 - 150 nmol/L (40-60 ng/ml) and recognize that levels of >200 nmol/L (80ng/ml) are potentially toxic. So how much Vitamin D do you have to take to reach this level? Again this is controversial… The IOM bumped its recommended dietary intake from 400 to 600 IU for adults and for 800 IU for age >70 years. The maximum level was set at 4000 IU. Many, including us at Wellness Garage, think these recommendations are low. For those who have not been tested for Vitamin D, we recommend 2000 IU per day. For anyone taking doses greater than 5000 IU we also recommend testing. For those who can afford testing, we recommend getting tested during the winter December to February and adjusting your supplementation based on the results. Vitamin D testing is no longer a medically insured service in most parts of Canada due to the cost, especially when a simple one size fits all recommendation to supplement will likely help most people. We think this makes sense from a public policy perspective, at least until there is better evidence to support that supplementation itself prevents or reverses disease. We do think that individuals who are looking to optimize their health should test as there are simply too many variables to ensure that a standard dose of Vitamin D will put you in the optimal zone AND we feel that while the causal role of Vitamin D has not been proven for most conditions, it is one of the most important health indicators and the potential benefit of optimizing Vitamin D levels outweigh the negligible risks with supplementation when guided by testing. So if you skipped over most of this to find the answers to your questions - here is a quick summary:
|
AuthorDr. Brendan Byrne Categories
All
|

 RSS Feed
RSS Feed