|
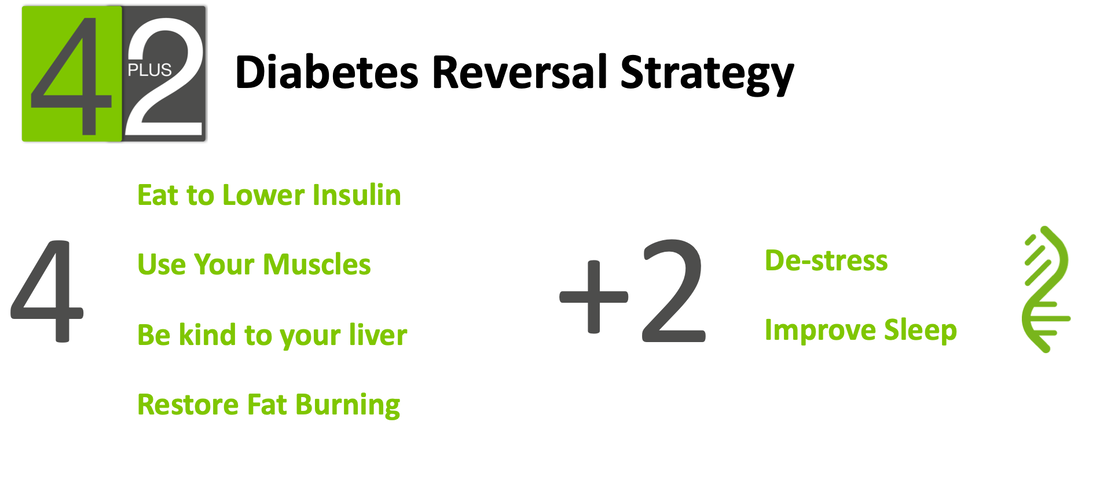
The 4+2 Diabetes Reversal Strategy programs are based on the research of Dr. Roy Taylor and his team in Newcastle over the past 20 years. Taylor has shown that Type II Diabetes is a disease of energy overload. Energy, from food, stored as fat, overwhelms our body’s healthy storage capabilities. Fat is then stored in places it shouldn’t be - within the cells of the liver, pancreas and muscle initially causing insulin resistance and eventually pancreatic beta cell dysfunction, abnormal blood sugars and diabetes. From cellular studies, to MRI imaging, all the way to a randomized controlled primary care study, Taylor developed the Twin Cycle Theory to explain the pathogenesis of Type II Diabetes and most importantly demonstrated the reversibility and potential for diabetes remission. Getting rid of the fat in the liver and pancreas, restores insulin sensitivity and improves beta cell function. The amount of fat in each organ is relatively small - 400g in the liver and only 5g in the pancreas. However to achieve these reversals most people need to lose significant weight. In the DiRECT study, Taylor and his colleagues showed that 86% of people who lost > 15kg of weight were able to achieve reversal of their diabetes. At Wellness Garage, we have taken these insights and combined them with other evidence to develop the 4+2 Diabetes Reversal Strategy with a goal of helping people reverse their Type II Diabetes. The 4+2 Diabetes Reversal Strategy consists of four key and two secondary behaviours: Our programs for patients have three phases:
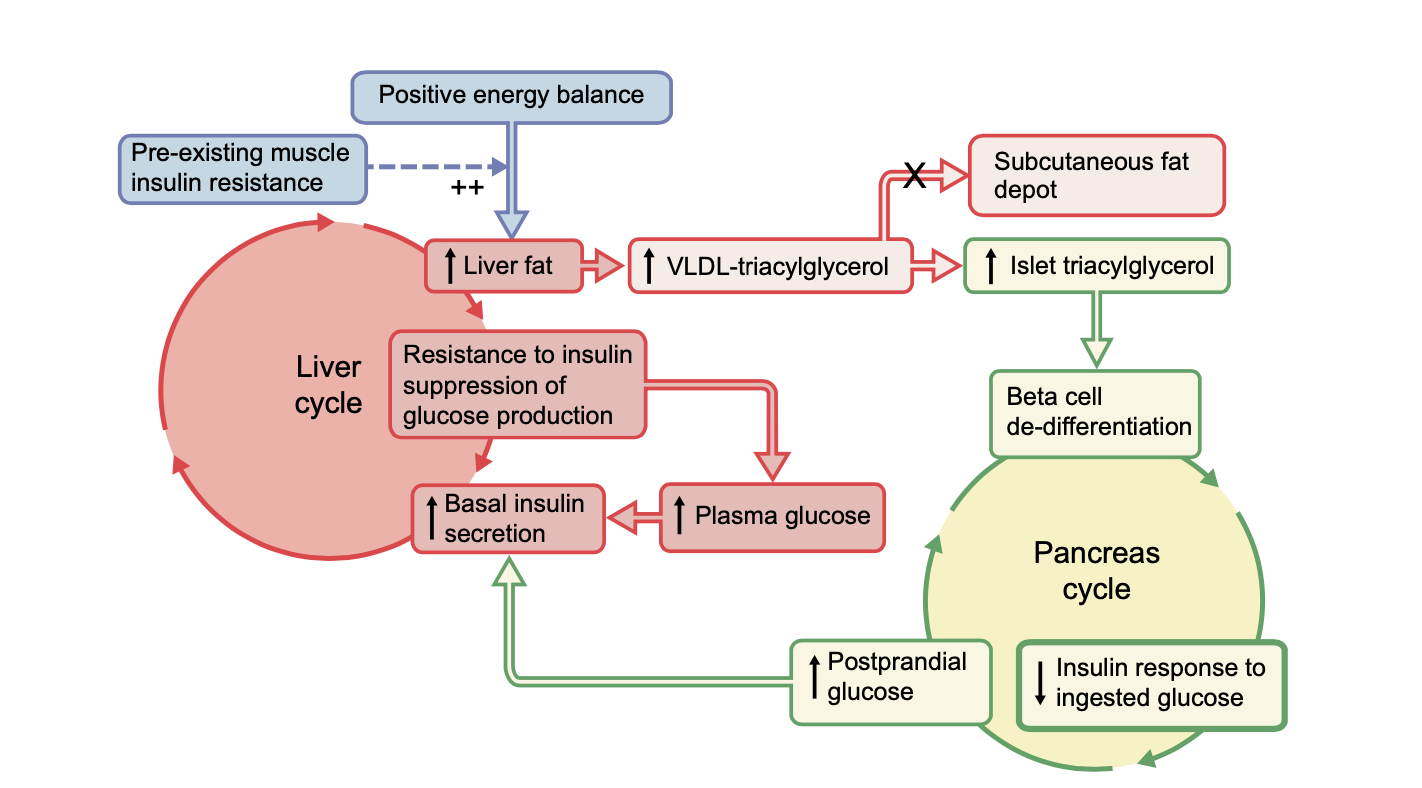
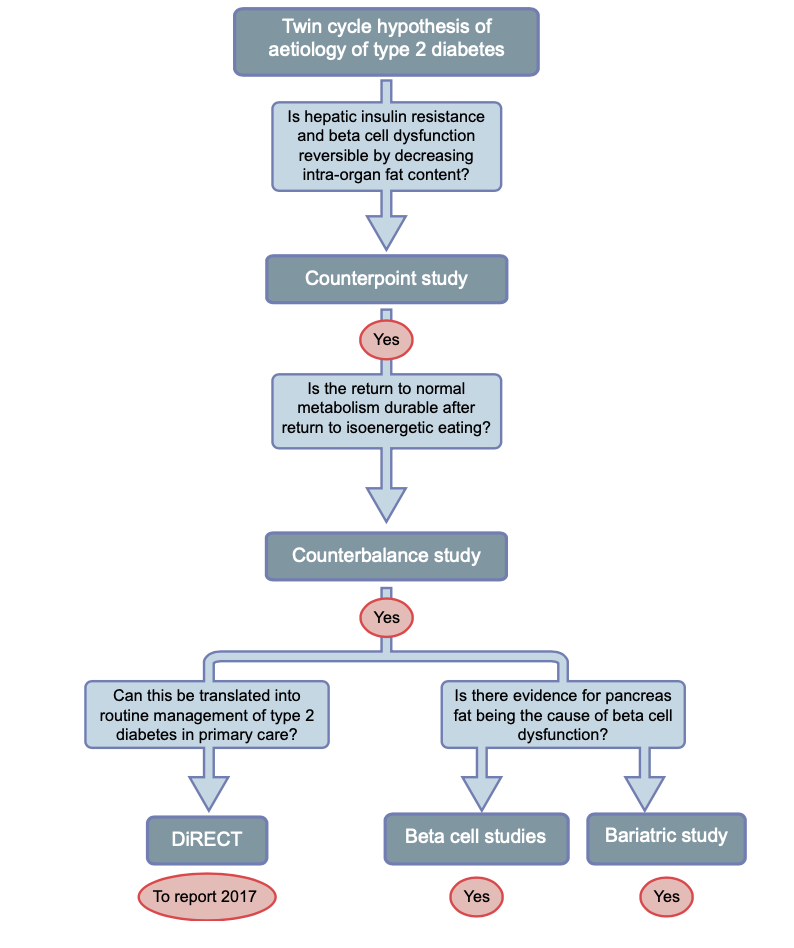
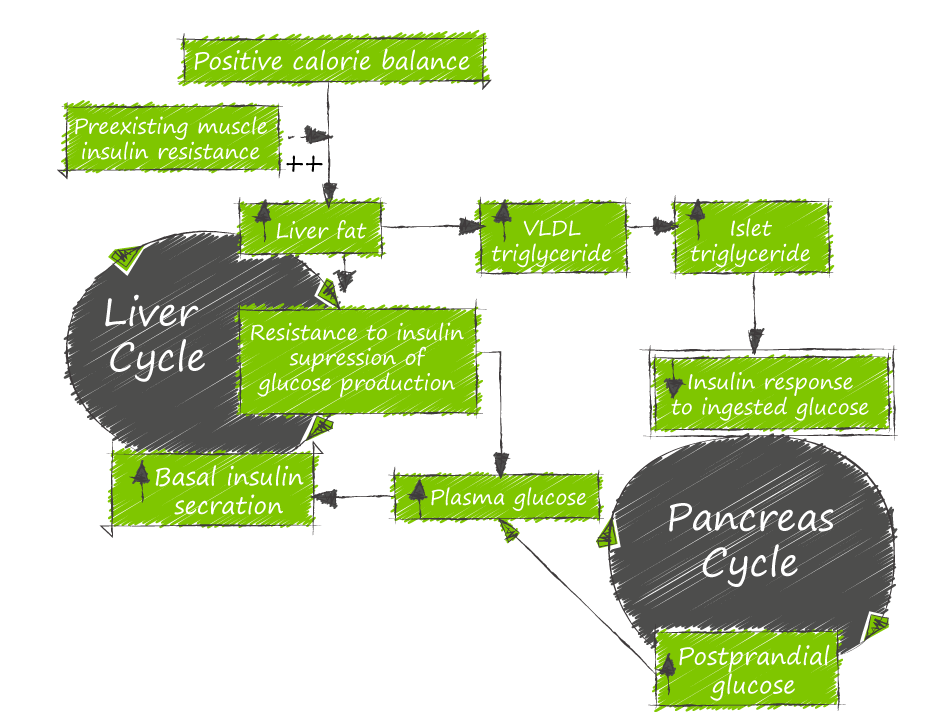
Research References: Taylor and team demonstrated that metabolic vicious cycles operating in the liver and pancreas (Twin Cycle) cause insulin resistance and beta cell dysfunction that results in Type II Diabetes AND that these processes can be reversed. They have systematically tested and confirmed each step of the hypothesis.
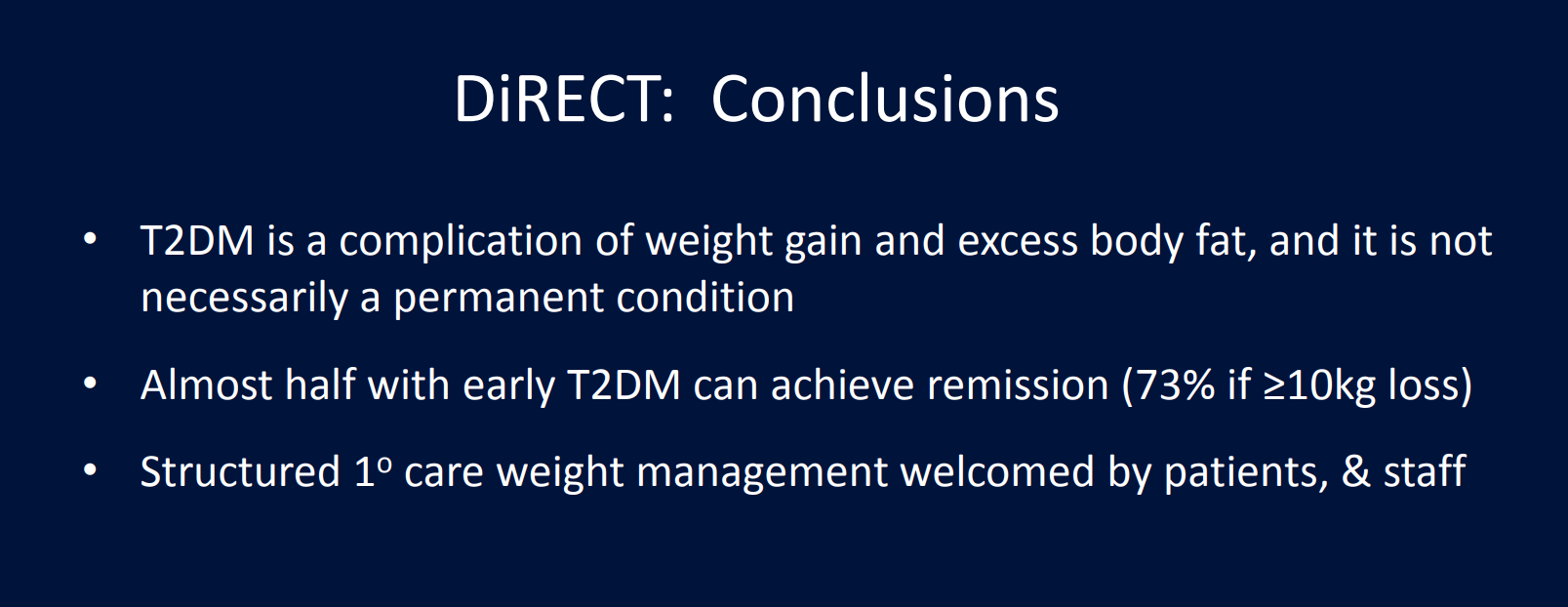
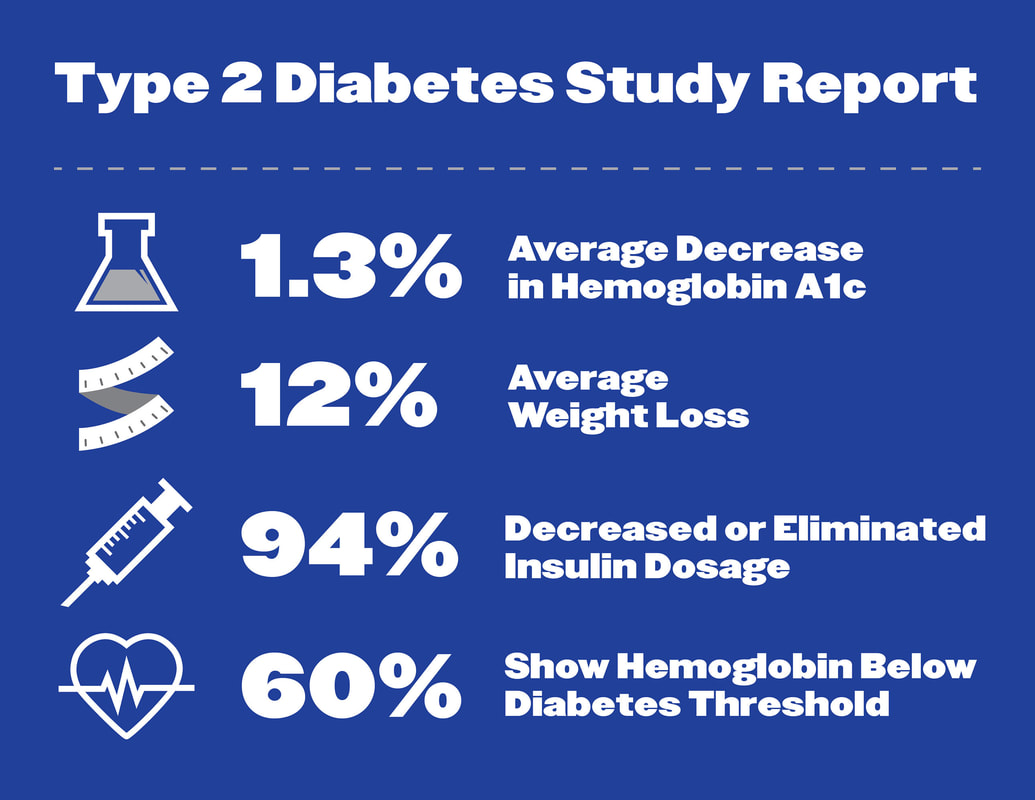
Last week, we detailed the process of insulin resistance and how Type II Diabetes develops. Diabetes is a disease of sustained energy overload that develops over many years. The body’s normal energy buffers gradually become overwhelmed, and stored energy in the form of fat disrupts the normal function of key organs. This disruption through a process called insulin resistance, creates a vicious cycle where energy once stored cannot be accessed, and the energy overload is perpetuated through hunger and increased appetite. Eventually, fat stored in the pancreas overwhelms the body’s ability to maintain normal blood sugars and the diagnosis of diabetes is made. On average it takes 10 to 15 years for this process to unfold. So the logical question arises - can we reverse this process? The short answer is yes. The first line of evidence for this comes from bariatric surgery, where as long ago as 1992 studies showed that between 30 and 70% of diabetes can be reversed for over 10 years. In more recent years, Dr. Susan Hallberg and her team at Virta Health, have shown reversal of diabetes through a dietary therapeutic intervention. Their results with a ketogenic diet, show that 60% of diabetics are in remission at the end of one year. Impressively, the population consisted of many individuals with longstanding diabetes as well as many taking insulin. Of those, 94% decreased dosage or eliminated insulin entirely by one year. From my perspective the most powerful research has come out of the UK from Dr. Roy Taylor and his colleagues in Newcastle. Through a series of clinical trials, culminating in the DIRECT study. They systematically showed that insulin resistance correlates and is caused by fat in the liver in the liver, and the development of abnormal blood sugars and diabetes correlates and is caused by fat in the pancreas. Eliminating the fat in the pancreas can restore the body’s ability to release enough insulin after eating and eliminating the fat in the liver restores the body’s ability to maintain normal fasting blood sugars. So how much fat do you need to lose in order to reverse diabetes? If you had a magic wand and could eliminate fat directly from the pancreas and liver you would only need to eliminate less than 1 pound - as it is estimated that the amount of excess fat in the liver is approximately 400g with even less ectopic fat in the pancreas. Taylor’s group estimates that even as much as 1ml or 0.6g of fat reduction from the pancreas is enough to restore pancreatic insulin secretion in patients that respond to weight loss. Of course, the challenge is that we do not have a magic wand so we must seek to lose weight and trust that some of it will come from the fat stored in our liver and pancreas that is causing our insulin resistance and diabetes. The DIRECT study was a randomized clinical trial (the highest source of clinical information) that demonstrated that 86% of patients that lost at least 15kg were able to put their diabetes into remission. The therapeutic intervention was a hypocaloric diet (830 calories per day) provided by meal replacements. Further research by Taylor has shown that patients that subsequently slipped back into diabetes regained pancreatic fat. Common to all three lines of evidence, the degree of diabetes reversal correlates directly with the amount of weight lost. So the evidence is clear that diabetes can be reversed provided you can lose enough weight and keep it off. It’s that last bit - and keep it off that is problematic. The challenge with using a diet to lose this weight is that diets do not work over the long term. Temporary restrictive approaches - whether it be of calories (DIRECT study) or carbohydrates (VIRTA Health) are prone to regression. The only way to get long term results is through a behavioral approach. Change habits in order to achieve sustainability. The 4+2 Diabetes Reversal Strategy is built on this behavioral change model, incorporating an understanding of the physiology of insulin resistance and Type II Diabetes.
Step 1: Eat to Lower Insulin Decrease insulin requirements by decreasing the intake of simple and refined carbohydrates. Replacing refined foods with whole foods with a special focus on fibre will result in less insulin required to maintain blood sugars. Pairing fibre rich, low glycemic, whole food carbohydrates with adequate protein and healthy fats helps normalize blood sugars after meals and provide steady glucose supply from food for hours. Step 2: Use Your Muscles Recognizing the role of skeletal muscle as the key energy buffer for glucose; the next part of the 4+2 Diabetes Reversal Strategy is to leverage exercise and activity to increase the uptake of glucose from meals into muscle. This uptake in turn decreases the amount of glucose converted to fat by the liver. Step 3: Be Kind to the Liver The ability to maintain blood sugars while fasting is dependent on the liver making glucose from glycogen or other sources (gluconeogenesis). Fat in the liver causes insulin resistance and results in the liver over-producing glucose with a corresponding elevation in fasting blood sugar. Decreasing fat in the liver is necessary to reverse diabetes, therefore decreasing fructose and alcohol - two substances that are directly metabolized into fat in the liver is essential. In addition, focusing on gut health with adequate fibre intake has been shown to improve liver function. Step 4: Restore Fat Burning The first three steps create conditions that improve metabolic flexibility and allow the body to burn fat, but at the end of the day ‘less calories in, than calories out’ is necessary to lose weight. One of the most effective behavioral approaches to weight loss is time restricted eating starting at 12 hour of fasting and increasing to 14 to 16 hours as tolerated. Time restricted eating works because it eliminates nighttime snacking and results in fewer calories consumed making a deficit more likely. It also improves metabolic flexibility and the use of fat as fuel when fasting. When this is done after the first three steps, it is generally very easy to incorporate with minimal hunger symptoms. The +2 in the Diabetes Reversal Strategy involves decreasing the negative effects of cortisol on insulin sensitivity. Step 5: De-stress Finding ways to bring down cortisol without resorting to calories improves our ability to lose weight. Techniques as varied as meditating, yoga, time in nature and pursuing your hobbies have been shown to dissipate stress and bring cortisol levels down. Step 6: Improve Sleep Inadequate sleep elevates cortisol and appetite, often driving poor food choices (ie. comfort foods high in both fat and simple carbohydrates). Studies clearly show that adequate sleep can reset our stress mechanisms resulting in lower cortisol levels and improve appetite control. The 4+2 Diabetes Reversal Strategy works at the behavioral level to gradually and systematically shift to new healthy habits that are sustainable for the long run. Over time, blood sugars are better controlled, medications are reduced, weight is lost and diabetes is reversed. There is no magic to this - just sound evidence-based behaviours supported by science. At Wellness Garage we have developed a number of programs to support people who want to take control of their health and reverse diabetes: Our 4+2 Diabetes Reversal Group sessions are MSP funded group medical visits designed to provide you with all the information you need. Our 1:1 Coaching Program provides you with individualized nutrition, exercise and health coaching support to guide you to your own reversal path. “How did you go bankrupt?” Bill asked. “Two ways,” Mike said. “Gradually and then suddenly.” Ernest Hemingway, “The Sun Also Rises" Like Hemingway’s description of bankruptcy, Type II Diabetes develops gradually and then suddenly. Diabetes is a disease of sustained energy overload that develops over many years. The body’s normal energy buffers gradually become overwhelmed, and stored energy in the form of fat disrupts the normal function of key organs. This disruption through a process called insulin resistance, creates a vicious cycle where energy once stored cannot be accessed, and the energy overload is perpetuated through hunger and increased appetite. Eventually, fat stored in the pancreas overwhelms the body’s ability to maintain normal blood sugars and the diagnosis of diabetes is made. On average it takes 10 to 15 years for this process to unfold. To understand diabetes we need to understand how our body is designed to manage energy. Energy comes from food. Specifically the fats, carbohydrates and proteins that make up the food we eat. Our bodies have two different and related ways to store energy from food: glucose and fat. Glucose is the preferred fuel for our brains and converts to energy faster in our muscles, but it has two major limitations:
Our brain’s consume 1 tsp of glucose per hour and at rest the rest of the body consumes 1 tsp per hour. In other words, our blood glucose is turned over twice per hour. This glucose is supplied directly from food when we are eating and absorbing meals and from stored glucose (glycogen) when we are fasting. Our livers can only store about 150g of glycogen - for perspective this represents only 15 hrs of basal glucose production (150g = 30 tsp = 15 tsp @ 2 tsp/hr). Fortunately our livers can also make glucose from fat, protein and lactate (broken down from muscle glycogen). So our livers are constantly trying to maintain blood sugar levels by either breaking down glycogen (glycogenolysis) into glucose or breaking other compounds (gluconeogenesis). These processes are both controlled by the pancreas through the release of two hormones:
Fat is our slow fuel and we have unlimited capacity for storage. Each gram of fat has 9 calories vs the 4 calories in a gram of glucose and fat can be stored as triglycerides (3 fatty acids linked to a glycerol backbone) without water. So for each day of stored energy we only need to carry 278g or 0.6 lbs. While fat is a slower fuel, in that it takes more time to liberate its energy, many cells with a steady basal energy requirement prefer fat as fuel - heart, intestines, muscles (at low levels of activity). When we eat food, the digestive process breaks it down into its basic components. Fat is broken down into fatty acids which are absorbed, reassembled as fats and distributed to cells that use fat for energy and stored in adipose (fat) tissue. Proteins are broken down into amino acids, distributed to cells that need them and then converted into fat or glucose by the liver depending on our energy needs. Carbohydrates are broken down into glucose, absorbed into the bloodstream triggering the release of insulin from the pancreas. 80-90% of glucose will be stored in the muscles as glycogen, 10% stored in the liver as glycogen with anything extra converted by the liver into fat. So when we eat, we use carbohydrates to top up our glycogen stores and store everything extra as fat. When we are not eating we break down fat into fatty acids providing fuel to the cells that prefer fat, and glycogen into glucose to maintain blood glucose at a steady state. This works well when we are in energy balance. Some days we store a bit more, some days we draw down a bit more. Both energy systems have buffers against overload. The glucose system has a small but immediate buffer through the storage of glucose as glycogen in muscle. The fat system has an immense capacity to buffer excess energy through the storage of fat in subcutaneous adipose tissue. And of course the fat system can buffer the glucose system. With prolonged periods of energy overload these buffers begin to break down. Muscle inactivity results in lower capacity to store glycogen in muscle resulting in more energy being converted into fat. Our ability to store fat in subcutaneous tissue eventually hits a limit. This limit differs greatly amongst different people and is known as the personal fat threshold. We have two ways to store extra fat - store more fat in existing fat cells or create more fat cells. By the time we are 2 years old the number of our subcutaneous fat cells is set. So once these cells are full we have to store fat elsewhere. We retain an ability to create new fat cells in our abdominal space around our intestines and other organs (viscera). This visceral fat is a further attempt to buffer energy overload but it is not without cost, as these fat cells send out inflammatory signals activating our immune system. Fat also begins to build up in other non-fat cells (ectopic fat). As fat builds up in these cells, their ability to respond to insulin decreases; they become insulin resistant. Ectopic fat in muscle results in insulin resistance and muscle takes up less of the glucose from dietary carbohydrates; causing more of this glucose to be converted to fat in the liver. Ectopic fat in the liver also results in insulin resistance. The pancreas initially responds to this insulin resistance by pumping out more insulin both in response to meals but also at baseline to control the liver’s production of glucose in order to maintain normal fasting blood sugars. This increased basal insulin level suppresses the body’s ability to utilize fat for energy as one of insulin’s effects is to inhibit fat oxidation. At this point, weight gain becomes inevitable further compounding the issue. Food is eaten, food is stored, but high levels of insulin prevent the utilization of that stored energy and hunger mechanisms are triggered resulting in more food intake. This extra food energy is in turn stored and the overloaded fat storage system continues to find new, but unhealthy places to store fat: visceral and ectopic fat. This vicious cycle repeats and the problem progresses. Eventually, ectopic fat finds its way into the pancreas and affects insulin production. At this point, insulin production plateaus and can no longer control blood glucose levels. By the time that blood sugars begin to rise - insulin levels are 2-3 times normal levels and 50% of pancreatic beta cells (cells that produce insulin) are dysfunctional. Once fasting blood sugars reach 7.0 mmol/L we call this Type II Diabetes and an estimated 80% of pancreatic beta cells are no longer secreting insulin. The path to Type II Diabetes is the result of sustained energy overload systematically overwhelming our body’s buffers - muscle for glucose and subcutaneous adipose tissue for fat. Over time, excess energy becomes stored as fat in places that it should not be - visceral fat in the abdomen and ectopic fat in cells throughout the body. This fat worsens insulin resistance, resulting in higher insulin levels, and decreasing our ability to use the stored energy driving hunger that adds more energy to an overloaded body. Our individual propensity toward insulin resistance and its manifestation as Type II Diabetes is variable and dependent on such factors as age, genetics, obesity, especially visceral obesity, sedentary behavior, stress, poor sleep and of course poor nutrition.
Learn more about our Diabetes Reversal Programs Previous blog posts: Diabetes Reversal Part I Diabetes Reversal Part II Diabetes Reversal Part III In Part I of this series, we reviewed the extent and impact of the diabetes epidemic and noted that the traditional approach to diabetes was clearly not working to prevent or reverse diabetes. In Part II, we dove into the science to show that we have had evidence that Type II Diabetes could be reversed through bariatric surgery. What was most interesting was the fact the improvements in blood sugar control and diabetes emerged well before the weight loss resulting from the surgery. The trigger theory of the twin cycle postulates a mechanism behind this dramatic and immediate improvement and suggests a path where therapeutic diet interventions could accomplish the same effects as bariatric surgery. From this theory, the key to diabetes reversal lies in improving liver function and decreasing the liver’s role in diabetes by changing the fat flows from the liver - the key steps:
Here the evidence is mixed between evidence from diets of varying: The DIRECT study (http://www.directclinicaltrial.org.uk) in the UK - took 298 Type II diabetics people through a randomized controlled study:
The results were dramatic:
VIRTA Health has recently (https://www.virtahealth.com) research published the 1 year results of their study of 300 Type II Diabetics
What is interesting is the difference in composition of the VIRTA diet:
The VIRTA study included longstanding diabetics and those on insulin while the DIRECT study spefically excluded these populations. Both studies clearly show that therapeutic nutritional intervention can reverse diabetes. In both studies, changes in blood sugars came before weight loss and correlated with changes in liver function - suggesting similar mechanisms: reducing the metabolism of carbohydrate into fat by the liver, and reversing the flow of fats from storage to utilization. In my opinion, the biggest practical difference between these approaches is calorie restriction vs carbohydrate restriction and which is easier to sustain over time. This is where a ketogenic approach may have advantages. It has been proposed that there is a metabolic advantage to ketosis whereby a 'calorie is not a calorie'. In other words ketogenic diets cause a greater expenditure of energy than non-ketogenic diets. Scientific evidence for this is limited, and if there really is an advantage, the effect is likely small and would not explain why people lose weight when carbohydrates are restricted to the point of ketosis. This common observation of sustainable weight loss with ketosis is more likely explained by three attributes of nutritional ketosis:
Bottom Line:
How can these findings be applied to diabetics today?
Learn more about the Wellness Garage 4+2 Diabetes Reversal Strategy Programs Other Blog Posts in this Series: Is Diabetes Reversible - Part I Is Diabetes Reversible - Part II In part I, we discussed the impact of Type II Diabetes on our health and the extent of the epidemic of diabetes in Canada and the world:
The traditional approach can be summarized as:
Yet we have clear evidence that diabetes can be reversed. The first hint of this reversal comes from the outcomes of bariatric surgery. In 1992, Pories et al. showed that blood glucose levels normalized in obese people with Type 2 diabetes who had undergone bariatric surgery and that almost 10 years later 90% remained free of diabetes. The effect of bariatric surgery to reverse diabetes has been replicated in numerous studies with rates of remission ranging from 30 to 70% depending on the procedure and trial. Overall the long term remission correlates with the amount of fat loss achieved and maintained. But this correlation may be misleading when it comes to causation. The changes in insulin resistance and blood sugar happen well before there is any significant loss of fat. Initially there was belief that these early effects were mediated through incretin hormone secretion. Closer analysis shows that real change happens through the initial rapid decline in caloric intake at the time of surgery. This creates a sudden reversal of traffic into fat stores that brings about a profound change in the intracellular concentration of fat metabolites. This effect happens first in the liver and other ectopic (visceral) fat storage sites. These changes represent a sudden and dramatic reversal of the proposed cause of insulin resistance. With this evidence that Type II DM can be reversed by bariatric surgery and that the effect results from the immediate reversal of the intracellular changes that cause insulin resistance and diabetes in the first place, the next question is can this be done through diet - without the cost, risk and complications of surgery. The simple and resounding answer is YES: Type II DM can be reversed through dietary interventions. Before we look at the therapeutic nutrition trials that are now providing evidence that diabetes is reversible, I want to step back and look at the mechanism and time course of insulin resistance, as this will help us understand what approach an individual looking to reverse diabetes should follow. Insulin resistance is a process by which muscle, fat and liver cells no longer respond properly to insulin and thus cannot easily absorb glucose from the bloodstream. As a result, the body needs higher levels of insulin to help glucose enter cells. The liver is the key player in the development of diabetes, as it is the hepatic production of triglycerides from excess carbohydrates that is at the root of the disease process. Interestingly, it is the reversal of insulin resistance in the liver that occurs during the immediate hypocaloric response to bariatric surgery. The trigger theory for the twin cycle explains the mechanism for both the development and reversal of Type II DM, and provides the foundations of a strategy for a new paradigm for diabetes management. This theory postulates that:
These changes in the liver also lead to
The key is to understand at what the point the trigger is activated in the liver, that is the point at which liver fat accumulates along with the corresponding trigger level at which adverse metabolic effects of fat on the pancreas occur. The goal of any therapeutic effort to reverse diabetes would then be to reduce the liver and pancreas fat below the personal trigger levels. The key here is the liver: we have known for some time that insulin resistance in Type II DM correlates with liver fat - decrease the liver fat and the diabetes improves. How do we decrease liver fat?
If bariatric surgery’s immediate effect on diabetes results from this hypocaloric induction – can this be done through diet alone, without surgery. In Part III, we will explore some of the new and powerful evidence for therapeutic nutrition that demonstrates that Type II Diabetes is in fact reversible through dietary interventions. Is Diabetes Reversible - Part I Is Diabetes Reversible - Part 3 In medical school we were taught that Type II DM is a chronic progressive disease - once diagnosed, it could potentially be managed, controlled, but never cured. The primary thrust of diabetic cares has been to try and control blood sugar with a goal of decreasing the risk of macrovascular (heart attack and stroke) and microvascular (kidney failure and blindness). Conventional wisdom has been that 90% of diabetics require medication treatments that need to intensified over time to effectively prevent complication and that "delays in intensification of are common and may be due to unrealistic patient expectations." (1) Evidence is accumulating that conventional wisdom has been wrong. The Massive Toll of Diabetes Diabetes rates globally are rising, driven by the obesity epidemic.
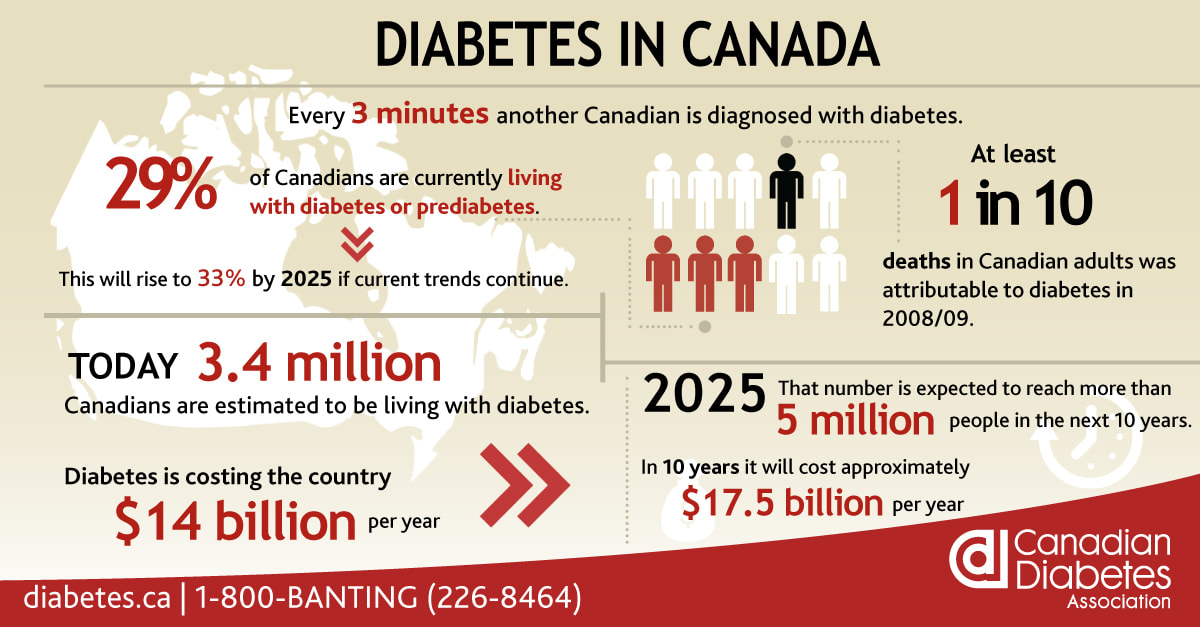
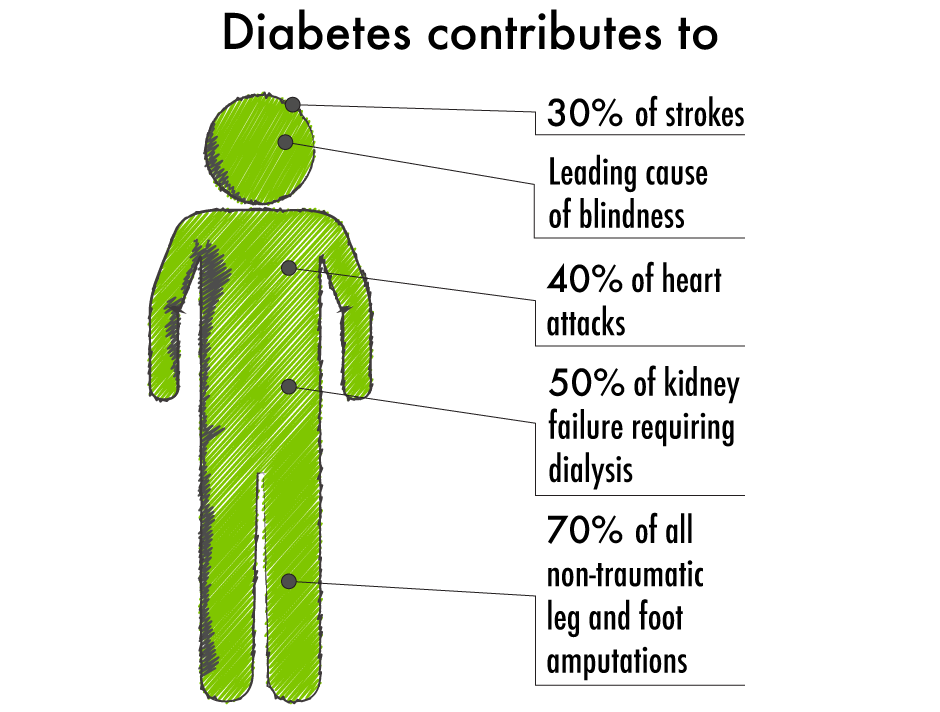
In Canada, 9% of the population is diabetic - this has grown from 3.3% in 1998 and is expected to grow to 12% in 2025. Perhaps even more alarming, an additional 22% of the population are pre-diabetic, 90% of whom do not realize it. Over 70% of pre-diabetics will go on to develop diabetes. Diabetes reduces lifespan by 5-15 years and accounts for over 10% of deaths in Canadian adults. People with diabetes are:
Diabetics have a 25% greater chance of developing cancer. Diabetes is moderately associated with cancers of the:
Diabetes and depression create a self-enforcing viscous cycle: 30% of diabetics have clinically relevant depressive symptoms, people with depression have a 60% increased risk of developing type 2 diabetes. Adding to this massive clinical toll, the cost of diabetic care is staggering - in Canada we currently spend $15B on treatment and management of complications. With the rates of diabetes climbing the cost trend has been called an economic tsunami, with an expected doubling by 2025. Looked at from both the clinical and financial perspective, it is clear that diabetes is the biggest healthcare challenge of our generation. Stepping back, we can see that our traditional approach:
... is not working, for the simple reason: our current approach does not address the cause of diabetes. The chronic and progressive nature of diabetes may have more to do with our management than of the disease itself. In part II and III of this blog series, I will look at the powerful new evidence that Type II Diabetes can be reversed through a comprehensive lifestyle approach. At Wellness Garage, we believe that the answer to optimal health and vital longevity lies in our lifestyle behaviors. We use comprehensive, evidence-based, precision health assessments to gain deep understanding of an individuals current health and behaviors. We then use this information to come up with a behavioral plan to address underlying illness and risk, while optimizing health. If this approach makes sense to you, learn more about our 4+2 Diabetes Reversal Strategy programs Is Diabetes Reversible - Part II Is Diabetes Reversible - Part IIII Understanding Insulin Resistance is the First Step to Reversing Diabetes How to Reverse Diabetes 50% of Americans have high blood pressure according to the new guidelines from American College of Cardiology and the American Heart Association. Lost in the debate about whether this makes sense to label so many people with a disease was the recognition that normal blood pressure is now defined as 120/80 and the acknowledgement that the risks from blood pressure increase progressively, and linearly from levels as low as 115/75 in people from 40 to 89 years of age. For every increase of 20 mmHg systolic and 10 mmHg diastolic there is a doubling of mortality from both heart disease and stroke. Here is the Wellness Garage strategy for high blood pressure: 1. Know your blood pressure:
2. Know whether you have insulin resistance:
3. Get moving - exercise is key
4. Eat better - lose weight
5. Salt - stop eating packaged food and decrease how much you eat out - see #3
7. Sleep - develop a great sleep routine
This 7 step strategy will allow you to take control of your blood pressure and do everything you can to either avoid medication or take as little as possible. Backgrounder on Hypertension:
What is it?
How is it defined?
Why is it important?
What causes it?
Humans need to eat. Cells throughout the body are predominantly fueled by glucose delivered through the blood. In evolutionary times food was not predictable, most often scarce, sometimes abundant. To maintain a consistent energy supply of blood glucose, evolution created a complex signaling system to control the process, delivering glucose when it is needed and efficiently storing it, when calories are abundant, ready to be mobilized in times of scarcity. Two hormones are central to this signaling process: insulin and glucagon. When blood sugar drops, pancreatic alpha cells release glucagon which then triggers the release of glucose from the liver. Correspondingly, when blood sugars rise, pancreatic beta cells release insulin which promotes glucose uptake in the liver and muscle, storing it as glycogen initially and then when glycogen stores are maximized, insulin prompts the conversion of carbohydrates and proteins to fat, our most efficient way to store calories for the future. Both insulin and glucagon are small proteins recognized by specific receptors on individual cells. This process, developed over 600M years of evolution, now is under challenge in humans. The conditions for which we are optimized: calorie scarcity with intermittent abundance, no longer exist. Instead we live in a world of continuous excess calories, with processed foods that rapidly spike blood sugars and trigger massive insulin release, and correspondingly massive insulin directed storage of excess calories as fat in adipose tissue. For many this process has become a one-way street, the flexibility to shift metabolically from glucose to fat as fuel that was once the key to our survival has, for many people, been lost. They are dependent on maintaining blood sugars through the constant consumption of carbohydrates. - if you find yourself craving sweats, getting tired after eating and feeling generally fatigued - this could be happening to you. As a result of excess calories, sedentary lifestyles and this loss of metabolic flexibility, global levels of obesity are soaring: 2 Billion people are overweight - 650M are obese. In Canada close to 50% of the population is overweight!. With obesity has come a corresponding epidemic of obesity related diseases:
The cellular mechanisms by which insulin resistance manifests are complex and beyond the scope of this blog, but at a high level, dysfunctions in three areas appear to alone, or in combination affect the ability of insulin to efficiently activate the insulin receptor and trigger the cascade of reactions that allows insulin to do it's job:
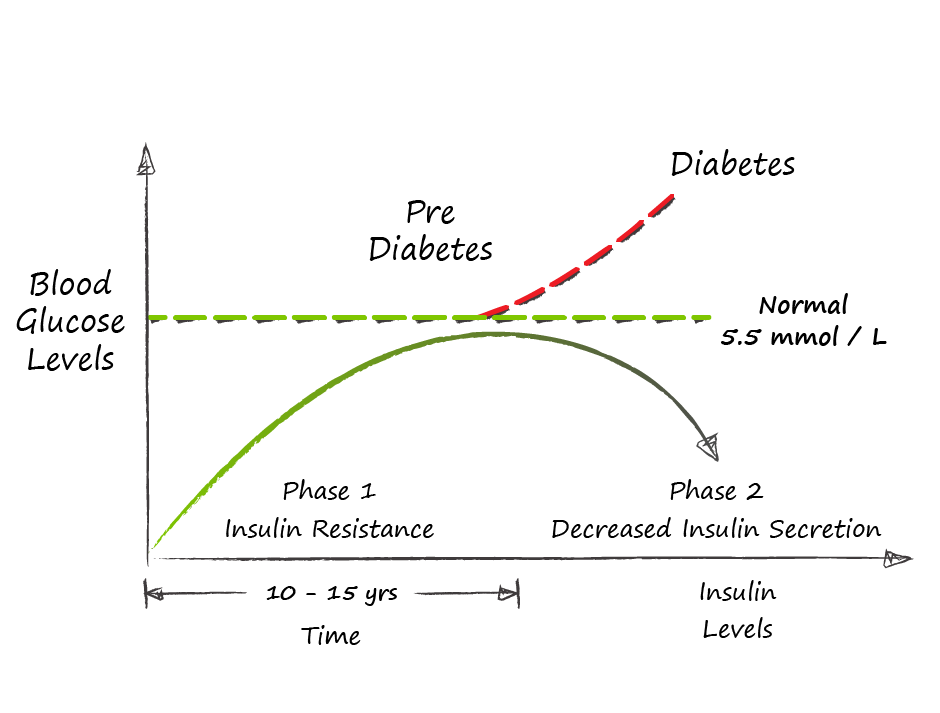
The process by which insulin resistance progresses to pre-diabetes and diabetes is understandable and predictable - it is also very preventable. As insulin resistance sets in, muscle, fat, and liver cells do not respond properly to insulin and thus cannot easily absorb glucose from the bloodstream. As a result, the body needs higher levels of insulin to help glucose enter cells. The beta cells in the pancreas try to keep up with this increased demand for insulin by producing more. As long as the beta cells are able to produce enough insulin to overcome the insulin resistance, blood glucose levels stay in the normal range. Over time, the processes that led to insulin resistance in the first place cause pancreatic beta cells to become less efficient and eventually triggers beta cell death. As this begins to happen, blood sugars fall out of the normal range and people begin to be diagnosed with pre-diabetes or diabetes on the basis of abnormal blood sugars. The time that it takes to progress from insulin resistance to pre-diabetes is generally in the order of 10-15 years - during this whole time a person will have normal blood sugars and may feel reassured that they do not have diabetes - YET - they are manifesting the underlying process of insulin resistance that will lead to diabetes and it's complications. So the big question that you should be asking is - how do I know whether I have insulin resistance? Direct testing of insulin response is not broadly available, so we are most often left looking for other signs of insulin resistance. For the most part, we can work with this:
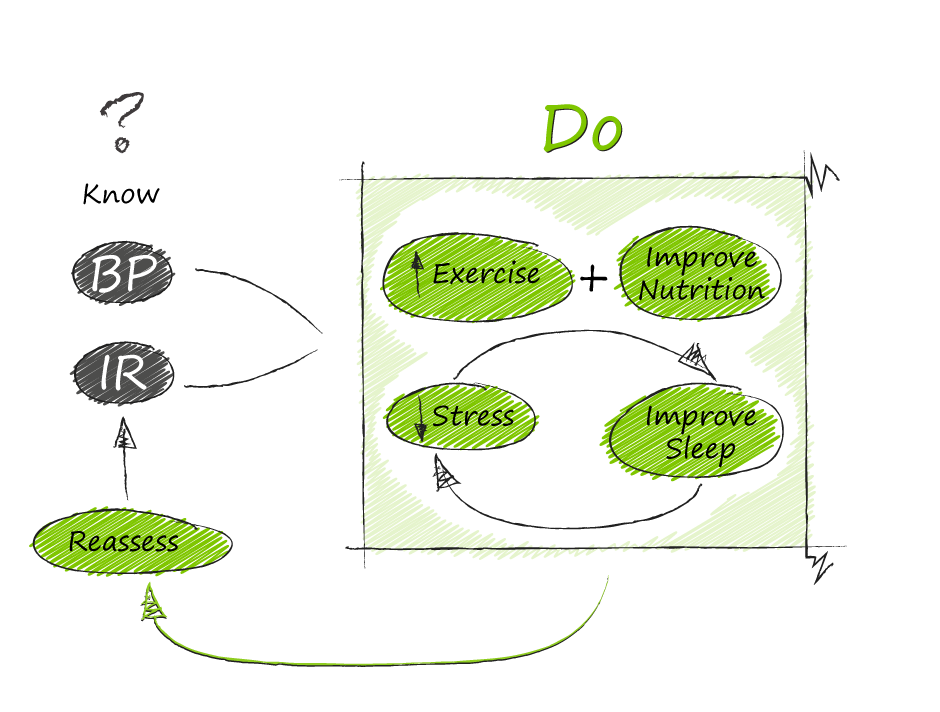
My blood sugars are normal, but I think I have insulin resistance, what do I do The good news is the process that leads to diabetes is reversible through lifestyle changes:
One of the major reasons we started Wellness Garage was to help people intervene early in preventable disease processes like insulin resistance rather than wait until blood sugars become abnormal (after 10-15 years!) and prescribe medications. If you think that you could be affected by insulin resistance - please reach out to us and book a free consultation, we can help you come up with a plan to address your health needs. |
AuthorDr. Brendan Byrne Categories
All
|





 RSS Feed
RSS Feed