|
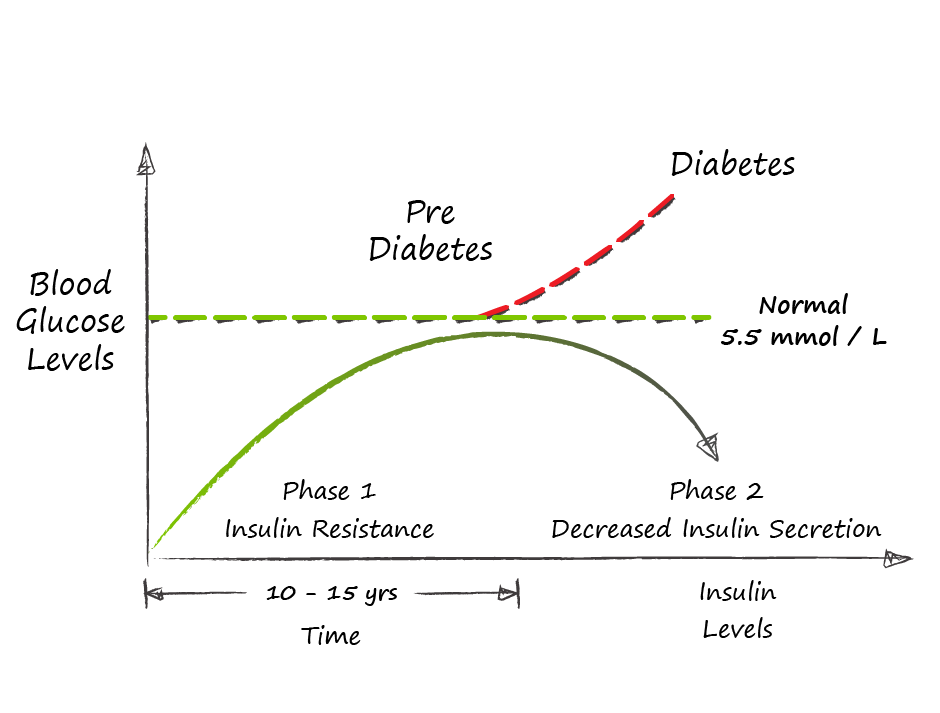
“How did you go bankrupt?” Bill asked. “Two ways,” Mike said. “Gradually and then suddenly.” Ernest Hemingway, “The Sun Also Rises" Like Hemingway’s description of bankruptcy, Type II Diabetes develops gradually and then suddenly. Diabetes is a disease of sustained energy overload that develops over many years. The body’s normal energy buffers gradually become overwhelmed, and stored energy in the form of fat disrupts the normal function of key organs. This disruption through a process called insulin resistance, creates a vicious cycle where energy once stored cannot be accessed, and the energy overload is perpetuated through hunger and increased appetite. Eventually, fat stored in the pancreas overwhelms the body’s ability to maintain normal blood sugars and the diagnosis of diabetes is made. On average it takes 10 to 15 years for this process to unfold. To understand diabetes we need to understand how our body is designed to manage energy. Energy comes from food. Specifically the fats, carbohydrates and proteins that make up the food we eat. Our bodies have two different and related ways to store energy from food: glucose and fat. Glucose is the preferred fuel for our brains and converts to energy faster in our muscles, but it has two major limitations:
Our brain’s consume 1 tsp of glucose per hour and at rest the rest of the body consumes 1 tsp per hour. In other words, our blood glucose is turned over twice per hour. This glucose is supplied directly from food when we are eating and absorbing meals and from stored glucose (glycogen) when we are fasting. Our livers can only store about 150g of glycogen - for perspective this represents only 15 hrs of basal glucose production (150g = 30 tsp = 15 tsp @ 2 tsp/hr). Fortunately our livers can also make glucose from fat, protein and lactate (broken down from muscle glycogen). So our livers are constantly trying to maintain blood sugar levels by either breaking down glycogen (glycogenolysis) into glucose or breaking other compounds (gluconeogenesis). These processes are both controlled by the pancreas through the release of two hormones:
Fat is our slow fuel and we have unlimited capacity for storage. Each gram of fat has 9 calories vs the 4 calories in a gram of glucose and fat can be stored as triglycerides (3 fatty acids linked to a glycerol backbone) without water. So for each day of stored energy we only need to carry 278g or 0.6 lbs. While fat is a slower fuel, in that it takes more time to liberate its energy, many cells with a steady basal energy requirement prefer fat as fuel - heart, intestines, muscles (at low levels of activity). When we eat food, the digestive process breaks it down into its basic components. Fat is broken down into fatty acids which are absorbed, reassembled as fats and distributed to cells that use fat for energy and stored in adipose (fat) tissue. Proteins are broken down into amino acids, distributed to cells that need them and then converted into fat or glucose by the liver depending on our energy needs. Carbohydrates are broken down into glucose, absorbed into the bloodstream triggering the release of insulin from the pancreas. 80-90% of glucose will be stored in the muscles as glycogen, 10% stored in the liver as glycogen with anything extra converted by the liver into fat. So when we eat, we use carbohydrates to top up our glycogen stores and store everything extra as fat. When we are not eating we break down fat into fatty acids providing fuel to the cells that prefer fat, and glycogen into glucose to maintain blood glucose at a steady state. This works well when we are in energy balance. Some days we store a bit more, some days we draw down a bit more. Both energy systems have buffers against overload. The glucose system has a small but immediate buffer through the storage of glucose as glycogen in muscle. The fat system has an immense capacity to buffer excess energy through the storage of fat in subcutaneous adipose tissue. And of course the fat system can buffer the glucose system. With prolonged periods of energy overload these buffers begin to break down. Muscle inactivity results in lower capacity to store glycogen in muscle resulting in more energy being converted into fat. Our ability to store fat in subcutaneous tissue eventually hits a limit. This limit differs greatly amongst different people and is known as the personal fat threshold. We have two ways to store extra fat - store more fat in existing fat cells or create more fat cells. By the time we are 2 years old the number of our subcutaneous fat cells is set. So once these cells are full we have to store fat elsewhere. We retain an ability to create new fat cells in our abdominal space around our intestines and other organs (viscera). This visceral fat is a further attempt to buffer energy overload but it is not without cost, as these fat cells send out inflammatory signals activating our immune system. Fat also begins to build up in other non-fat cells (ectopic fat). As fat builds up in these cells, their ability to respond to insulin decreases; they become insulin resistant. Ectopic fat in muscle results in insulin resistance and muscle takes up less of the glucose from dietary carbohydrates; causing more of this glucose to be converted to fat in the liver. Ectopic fat in the liver also results in insulin resistance. The pancreas initially responds to this insulin resistance by pumping out more insulin both in response to meals but also at baseline to control the liver’s production of glucose in order to maintain normal fasting blood sugars. This increased basal insulin level suppresses the body’s ability to utilize fat for energy as one of insulin’s effects is to inhibit fat oxidation. At this point, weight gain becomes inevitable further compounding the issue. Food is eaten, food is stored, but high levels of insulin prevent the utilization of that stored energy and hunger mechanisms are triggered resulting in more food intake. This extra food energy is in turn stored and the overloaded fat storage system continues to find new, but unhealthy places to store fat: visceral and ectopic fat. This vicious cycle repeats and the problem progresses. Eventually, ectopic fat finds its way into the pancreas and affects insulin production. At this point, insulin production plateaus and can no longer control blood glucose levels. By the time that blood sugars begin to rise - insulin levels are 2-3 times normal levels and 50% of pancreatic beta cells (cells that produce insulin) are dysfunctional. Once fasting blood sugars reach 7.0 mmol/L we call this Type II Diabetes and an estimated 80% of pancreatic beta cells are no longer secreting insulin. The path to Type II Diabetes is the result of sustained energy overload systematically overwhelming our body’s buffers - muscle for glucose and subcutaneous adipose tissue for fat. Over time, excess energy becomes stored as fat in places that it should not be - visceral fat in the abdomen and ectopic fat in cells throughout the body. This fat worsens insulin resistance, resulting in higher insulin levels, and decreasing our ability to use the stored energy driving hunger that adds more energy to an overloaded body. Our individual propensity toward insulin resistance and its manifestation as Type II Diabetes is variable and dependent on such factors as age, genetics, obesity, especially visceral obesity, sedentary behavior, stress, poor sleep and of course poor nutrition.
Learn more about our Diabetes Reversal Programs Previous blog posts: Diabetes Reversal Part I Diabetes Reversal Part II Diabetes Reversal Part III |
AuthorDr. Brendan Byrne Categories
All
|

 RSS Feed
RSS Feed